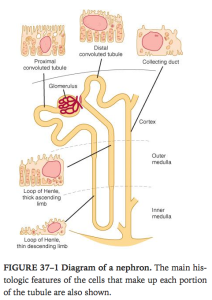
Review of anatomy of the nephron.
- Glomerulus + renal tubule
- Each kidney has 1.3million nephrons
- Cortical nephrons(85%) have shorter Loop of henle than juxtamedullary nephrons(15%)
- The ascending loop finishes with the specialised macula densa cells next to afferent more than efferent arterioles
- Macula densa + renin secreting juxtaglomerular cells = juxtaglomerular aparatus
- Proximal convoluted tubule – brush border, apical tight junction
- Collecting duct – Principal cells(Na reab and ADH related H2O reab) and intercalated cells(acid secretion and HCO3)
Vasa recta
Efferent arterioles from JG nephrons dive down next to the loop of henle to flow in a counter current which allows urine to be concentrated
Structure of the glomerulus.
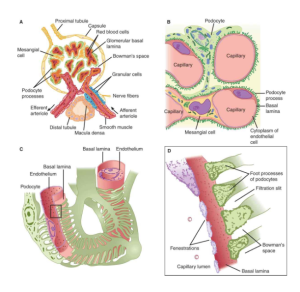
“A) Section through vascular pole, showing capillary loops. B) Relation of mesangial cells and podocytes to glomerular capillaries. C) Detail of the way podocytes form filtration slits on the basal lamina, and the relation of the lamina to the capillary endothelium. D) Enlargement of the rectangle in C to show the podocyte processes. The fuzzy material on their surfaces is glomerular polyanion.” Ganong’s Review of Medical Physiology, 24th Edition
- Blind end of renal tubule is the bowmans capsule which is invadinated by tufts of glomerular cappilaries
- Afferent and efferent arterioles
- Endothelium of glomerular endothelium is fenerstrated 70-90microm
- Podocyted have foot processes which wrap around capillaries – filtration slits(25nanom) closed by thin membrane
- Glomerular basement membrane
- Mesangial cells – located between basal lamina and endothelium -regulate glomerular filtration, involved in progression of glomerular disease, take up immune complexes and produce ECM.
Renal blood flow:
- Adults 1.2-1.3L/min = 25% of cardiac output
- Renal plasma flow and how measured.
- The amount of a substance excreted per unit of time divided by the renal arteriovenous difference as long as the amount in the blood is unaltered during passage through the kidney.
- Measured by Fick’s principle – uptake of a given substance per unit time/arteriovenous concentration difference across kidney
- Measured using p amino hippuric acid – plasma and urine
- Regulation of renal blood flow (including autoregulation).
- Noradrenaline – vasoconstricts renal arteries, afferent more than efferent
- Angiotensin II – vasoconstriction efferent more than afferent to maintain renal perfusion
- Dopamine – renal vasodilation and natriuresis
- Prostaglandins increase renal blood flow in cortex and decrease in medulla
- ACh – vasodilation
- High protein diet increases renal blood flow
- Nerves
- NA –> b agonist in JG cells –> renin release, then increased Na absorption, THEN vasocontriction (a agonist)
- Autoregulation
- The alteration of renal vascular resistance so renal perfusion is stable at a variety of vascular pressures
- Smooth muscle stretch response
- Angiotensin 2
- NO
GFR:
- 125mL/min, 10% lower in women
- How measured.
- Measure the excretion and plasma level of a substance that is freely filtered through the glomeruli and neither secreted nor reabsorbed by renal tubules eg inulin
- GFR = concetration of substance x urine flow / plasma concentration of substance
- Control of GFR.
- Size of the capillary bed
- Affected by contraction of mesangial cells
- Permeability
- Hydrostatic pressure gradient
- Osmotic pressure gradient
- Size of the capillary bed
Tubular function.
- These can be same, more(if tubular secretion) or less (tubular reabsorption) – difference is the net amount transferred
- Endocytosis
- Passive diffusion
- Active transport
- amount excreted = urine flow x urine concentration of substance
- Amount filtered = GFR x plasma concentration of substance
- Na+ handling.
- Reabsorption of Na and Cl is key in water homeostasis
- Na is paired to H, Glucose, amino acids, organic acids, phosphate, electrolytes
- Moves down electrical and concentration gradient into tubular epithelial cells then actively transported into interstitum by Na/K ATPase
- 60% of the filtered Na+ is reabsorbed in the proximal tubule, primarily by Na–H exchange.
- 30% is absorbed via the Na–2Cl–K cotransporter in the thick ascending limb of the loop of Henle
- 7% is absorbed by Na–Cl cotransporter in the distal convoluted tubule.
- 3%, is absorbed via the ENaC channels in the collecting ducts, and this is regulated by aldosterone
- Glucose handling:
- Reabsorbed in proximal convoluted tubule
- 100% reabsorbed
- 800mEq filtered
- SGLT – Na/Glucose goes down concentration gradient of Na on apical side
- The Glut 2 receptor transports Glucose into interstitum
- K+ handling
- 93.3% reabsorbed
- 90mEq excreted each day
- HCO3
- 100% reabsorbed
- Proximal Conv tubule
- Concept of renal threshold
- The plasma level at which transport maximum is exceeded and increased levels of a subtance starts appearing in urine eg glucose
- Splay.
- Deviation from ideal reabsorption curve
- The magnitude of the splay is inversely proportionate to the avidity with which the transport mechanism binds the substance it transports.
- PAH handling.
- Actively secreted into tubular fluid
- PAH secretion increases with plasma PAH concentration until max secretion rate is reached
- After this clearance rate drops.
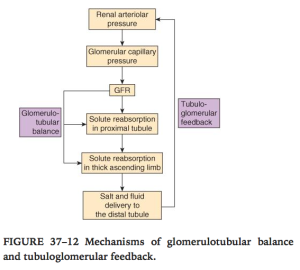
- Tubuloglomerular feedback
- Increasing Rate of flow through ascending LOH–> GFR at that nephron decreased
- Maintains constant load to DCT
- Sensor – macula densa –> adenosine release –> Ca release in smooth muscle cells of afferent arteriole–> vasoconstriction –> lowers EGFR
- Glomerulotubular balance
- The more that is filtered the more that is absorbed in proximal tuble (maintains percentage reabsorbed)
Viva questions:
- Tell me about the structure of the glomerulus.
- What is normal renal blood flow and how is it measured ?
- What is the normal renal plasma flow and how is it measured ?
- Tell me about the regulation of renal blood flow.
- Tell me about autoregulation in the kidney.
- Tell me about GFR and its regulation
- Tell me about sodium handling by the kidney.
- Tell me about glucose handling by the kidney.
- Tell me about potassium handling in the kidney
- Tell me about renal H+/HCO3- handling
- Tell me about renal water handling.
- What is tubuloglomerular feedback ?
- What is glomerulotubular balance ?
- Emptying of the bladder.
- What is the countercurrent mechanism