Chapter 4
EPSPs – excitatory post synaptic potential
- a temporary depolarization of postsynaptic membrane potential caused by the flow of positively charged ions into the postsynaptic cell as a result of opening of ligand-gated ion channels.
- Makes the cell more likely to fire an action potential
- Neurotransmitter – glutamate, acetylcholine
IPSPs – inhibitory post synaptic potential
- result from the flow of negative ions into the cell or positive ions out of the cell.
- Neurotransmitter- GABA
Generation of the A.P. in the postsynaptic neuron
- There is both excitary and inhibitory signals received
- The soma is an integrator of all the input
- Once the 10-15mV of depolarisation is reached, a propagated spike occurs
- In motor neurons the initial segment is the part of the cell with the lowest threshold for producing action potential – it is the area at and just beyond the axon hillock
- The AP travels down the axon and back to the soma to wipe it clean for the next potential
Inhibition & Facilitation
- Direct inhibition – inhibition that is not due to prev discharges of the post synaptic neuron eg in IPSP
- Indirect inhibition- difficulty firing due to the effects of prev discharges of the post-synaptic neuron
- In spinal reflex the afferent stimulates the agonist muscle and inhibits the antagonist muscle
- Pre synaptic inhibition which alters the ionic fluxes to inhibit action potentials and sometimes size of the potentials
- Eg: GABA – goes to GABA receptor–> increase Cl- conductance, increase K+ conductance –> decrease Ca2+ influx
- Pre synaptic facilitation is when Ca2+ channels are kept open for longer
Ach. & receptors
- Ach made in neurons, vesicle release needs synactobrevin
- Broken down in synapse by acetylcholinesterase, choline taken up by the nerve ending
- NMJ and CNS/autonomic ganglia- nicotinic receptors –> open Na channel when activated
- Smooth muscle and glands – Muscarinic receptors (increase IP3, DAG)–> secretions, miosis
Adr. / NorAdr. & receptors
- Tyrosine –> tyrosine hydroxylase –> DOPA (dihydroxyphenylalanine)–> DOPA decarboxylase–>dopamine–> dopamine beta hydroxylase –> noradrenaline –> phenylethanolamine methyltransferase –> adrenaline
- NA is at most sympathetic post ganglionic endings
- Locus ceruleus in brain
- NA is broken down by COMT and MAO
- adrenoreceptors are both are G protein coupled receptors–> inc cAMP
- Clonidine a2 agonist –> hypotension
Serotonin
(Important because of SSRIs etc.)
- Many 5HT receptor types – at least 7
- Found in platelets and GI tract (enterochromaffin cells) as well as brain.
- Made from tryptophan
- Reuptake
- Inactivated by mono amine oxidase in the cleft
- Urinary output of the break down product – 5 HIAA
GABA
- Major inhibitory transmitter in the brain
- Glutamate –> glutamate decarboxylase –> GABA
- GABA receptors – A, B, C, (C is mainly in retina)
- Ion channels
- GABA B is a G protein coupled receptor – increases K efflux,increase Cl- influx, inhibit adenyl cyclase, inhibit Ca2+ influx –> produce IPSP
Opioids & receptors
- Found in brain(analgesia) and GIT (decrease GI motility)
- Receptors – mu, kappa, delta – all three are G protein coupled and inhibit adenyl cyclase.
- Mu
- important in mediating analgesia, resp depression, constipation, euphoria, sedation, miosis, sedation
- increases K conductance and hyperpolarising
- Kappa and delta – closes Ca2+ channel
- Kappa
- Analgesia, diuresis, sedation, miosis, constipation, psychomimetic effects
- Delta
- Analgesia, neuro modulator release
Dopamine
- Nigrostriatal system – important in motor control
- Also broken down by COMT and MAO
Glutamate
- Main excitatory transmitter in brain and spinal cord
- NMDA receptors
Glycine
- Inhibitory neurotransmitter in Spinal cord
Neuro-muscular transmission
- Action potential reached end of nerve –> Ca2+ enters via voltage gated channels –> Acetylcholine released–> Ach binds to nicotinic receptors on muscle –> Na influx –>voltage gated Na channel open –> propagation of action potential in muscle.
Chapter 13
Organisation of Autonomic N.S.
- Sympathetic
- Parasympathetic
- Enteric
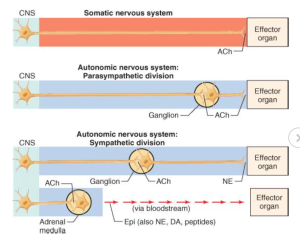
Comparison of peripheral organization and transmitters released by somatomotor and autonomic nervous systems
Motor neurons are A (large and myelinated), preganglionic neurons are B (small and myelinated) they then have 8 or 9 post ganglionic neurons each which are C fibres (small and unmyelinated).
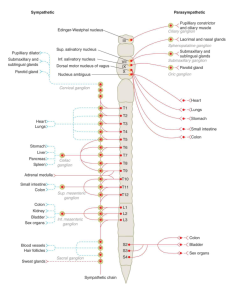
Parasympathetic
- Craniocaudal – cranial nerves + S2-S4
- Very short postganglionic neurons cos ganglion is very close to the organ
Sympathetic
- Thoraco Lumbar (T1-L3/4)
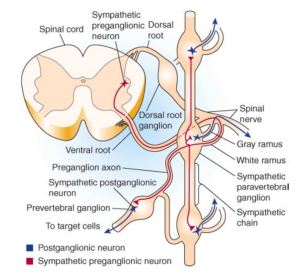
- Spinal cord –> Ventral root –> white ramus communicans–> paravertebral ganglion –> prevertebral ganglion(where post ganglionic nerve synapses) or back to spinal nerve via grey ramus communicans
Projection of sympathetic preganglionic and postganglionic fibers
Organization of sympathetic (left) and parasympathetic (right) nervous systems
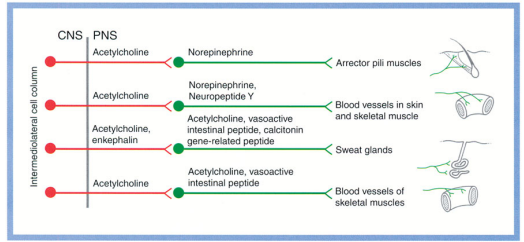
Autonomic neurotransmitters and their receptors/ effects
- All preganglionic neurons release ACh
- All parasympathetic postganglionic neurons release ACh
- Autonomic ganglia – Mediated by N2 nicotinic receptors (N1 at NMJ)
- Post ganglionic fibres – muscarinic receptors
| Alpha 1 agonist | Mydriasis, arteriolar constriction, venous contraction, sphincter contraction, decrease GI motility, uterine contraction, ejaculation, piloerection, sweating, thick viscous saliva |
| Alpha 2 agonist | arteriolar constriction, venous contraction, inhibit GI secretion, decrease GI motility, inhibit endocrine secretion |
| Beta 1 | Increase HR, increase contractility and speed of conduction, decrease GI motility |
| Beta 2 | increase contractility and speed of conduction, arteriolar dilation, venous dialtion, bronchial dilation, decrease GI motility, detruser and gall bladder relaxation, uterine relaxation |
Viva questions:
Chapter 4
- Describe cholinergic synaptic transmission.
- Describe adrenergic synaptic transmission.
- Describe neuromuscular transmission at the motor end plate.
- What are the different types of opioid receptors and their actions ?
- What is an EPSP / IPSP ?
- How is Ach. Synthesised / metabolised ? (Be able to discuss pseudocholinesterase)
- Describe the synthesis of catecholamines.
- How are catecholamines metabolised ?
Chapter 13:
- Describe the organisation of the Autonomic nervous system.
- Describe the distribution of cholinergic / noradrenergic / a1 / a2 / b1 / b2 receptors.
- What would be the effect of a cholinergic / adrenergic agonist / antagonist on the eye / heart / Peripheral vessels / lung / G-I system / bladder / skin etc.